It has been nearly nine decades since Sir Alexander Fleming’s accidental discovery of Penicillin at his Paddington laboratory in 1928, and today well over a hundred different types of antibiotics exist for numerous bacterial infections. A growing concern in modern medicine, however, is the ability of pathogenic bacteria to evolve strategies for overcoming antibiotic treatments. Many antibiotics such as ampicillin and erythromycin, for example, which used to kill off whole bacterial populations with great efficacy, are now capable of much less due to this alarming phenomenon of bacterial tolerance.
Researchers at Hebrew University in Jerusalem recently made an important discovery that advances our understanding of how bacteria are able to develop tolerance to antibiotics. Using the quantitative approach of physicists, they discovered that bacteria can quickly evolve to predict exactly when exposure to antibiotics will occur. As a result, the infectious bacteria will learn to lie dormant during the precise period of exposure, giving the population greater chance at survival.
Student invents world’s first bacteria-free food packaging
To illustrate this striking phenomenon, consider a patient taking antibiotics on a fixed schedule for some bacterial infection he had the misfortune to develop. Perhaps his doctor told him to take the antibiotics three times a day for ten days, spacing each dosage throughout the day at equal intervals. As this study indicates, the bacteria population may evolve after just a few days to modify its dormancy period to coincide with the duration of antibiotic exposure. To be sure, in the dormant stage nothing is absorbed by the bacteria, not even those “powerful” antibiotics.
A study on tolerance…for antibiotics
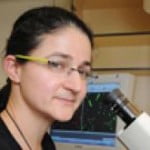
Professor Nathalie Balaban, a physics professor at Hebrew University’s Racah Institute of Physics, led the team of researchers, whose findings were published in last month’s issue of “Nature.” The main objective of their research was to gain a better understanding of the bacterial strategy to overcome antibiotic stress known as tolerance, which is not as well understood as the other adaptation strategy known as resistance. According to the literature, resistance enables a microorganism to continue growing while exposed to a specific antibiotic, whereas tolerance allows microorganisms to survive under antibiotic stress, regardless of the type of antibiotic present.
Prof. Balaban and her team hypothesized that a daily antibiotic dose of specific duration would enable the bacteria to predict delivery of the drug and lie dormant for that period in order to survive. To test this hypothesis, they exposed six populations of Escherichia coli, a bacteria, to repeated daily antibiotic exposures lasting 3, 5, or 8 hours, choosing ampicillin as their antibiotic.
In all cases, the bacteria remarkably adapted to their stressful regimens. Specifically, the lag time was found to be 3.4, 5.1, and 10 hours for the populations that evolved in response to daily 3, 5 and 8 hour exposures to antibiotics, respectively. The researchers were also able to prove that such an adaptation has a genetic basis.
Sign up for our free weekly newsletter
SubscribeOn top of this remarkable discovery, the researchers also observed a phenomenon regarding bacteria’s ability to adapt when antibiotic exposure is not predictable. In such an event, they noticed that the bacteria population, which is made up of millions of individual cells, will “hedge its bets” by spreading out the dormancy period among its cells as opposed to the entire population becoming dormant at the same time. That way, if a patient takes his antibiotics every 4-6 hours instead of every 5 hours on the dot, the population will still develop a certain tolerance level.
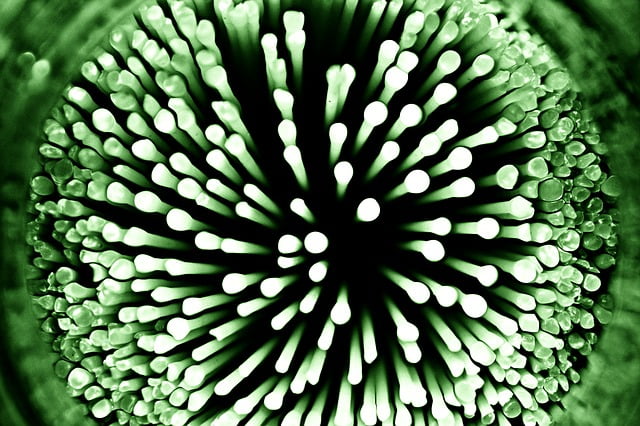
You won’t believe what this is
Waging a tougher war against bad bacteria
With this new understanding of how bacterial cells are able to evolve under antibiotic stress, scientists could develop better strategies for more effectively treating bacterial infections. Since the researchers were able to identify the genes responsible for the adaptation, the next step is to see whether or not the timed response to antibiotics is active in humans, too.
If the latter is found to be the case, it may explain the failure of antibiotic treatments observed in various diseases. In the future, it may help doctors to recommend different treatment schedules and it could also lead to the development of more efficient drugs.
Professor Nathalie Balaban, a physics professor at Hebrew University’s Racah Institute of Physics, led the team of researchers, which included colleagues from the Hebrew University’s Sudarsky Center for Computational Biology and the Broad Institute of Harvard and MIT. The ground-breaking research paper, “Optimization of lag time underlies tolerance in bacterial populations evolved under intermittent antibiotic exposure,” appears in the June 25 edition of the journal “Nature.”
Photos: Microbe World/ Hebrew University
Related posts

Israeli Medical Technologies That Could Change The World

Harnessing Our Own Bodies For Side Effect-Free Weight Loss

Missing Protein Could Unlock Treatment For Aggressive Lung Cancer



Facebook comments