Israeli researchers have helped to develop a new treatment combination for patients with advanced or metastatic head and neck cancer (HNC). The treatment, which uses both a targeted drug and immunotherapy following a certain sequence and within a specific time frame, blocks a signaling pathway that suppresses the immune system and keeps it from fighting tumor cells.
The research was conducted by an international team of scientists led by PhD student Manu Prasad in the laboratory of Prof. Moshe Elkabets of the Faculty of Health Sciences at the Ben-Gurion University of the Negev. Their findings were just published in the Journal for ImmunoTherapy of Cancer in a study co-authored by Israeli, Chinese, French, German, and US researchers.
The researchers targeted an aggressive type of HNC which is driven by the hyperactivation of a specific signaling pathway that will not allow the immune system to kill tumor cells. This was found in more than 40 percent of HNC cases.
Head and neck cancers include cancer in the larynx (voice box), throat, lips, mouth, nose, and salivary gland, or malignant tumors that arise from the lining of the head and neck regions.
The treatments currently available treatments are ineffective, Prof. Elkabets tells NoCamels. HNC develops in multiple sites on a person and existing treatments, which include chemotherapy, radiation, and immunotherapy have a relatively low response rate of about 20 percent. The average survival rate for patients in Stage III or IV of the disease is only about five years, says Elkabets. More so, even if patients are cured, 50 percent will eventually relapse.
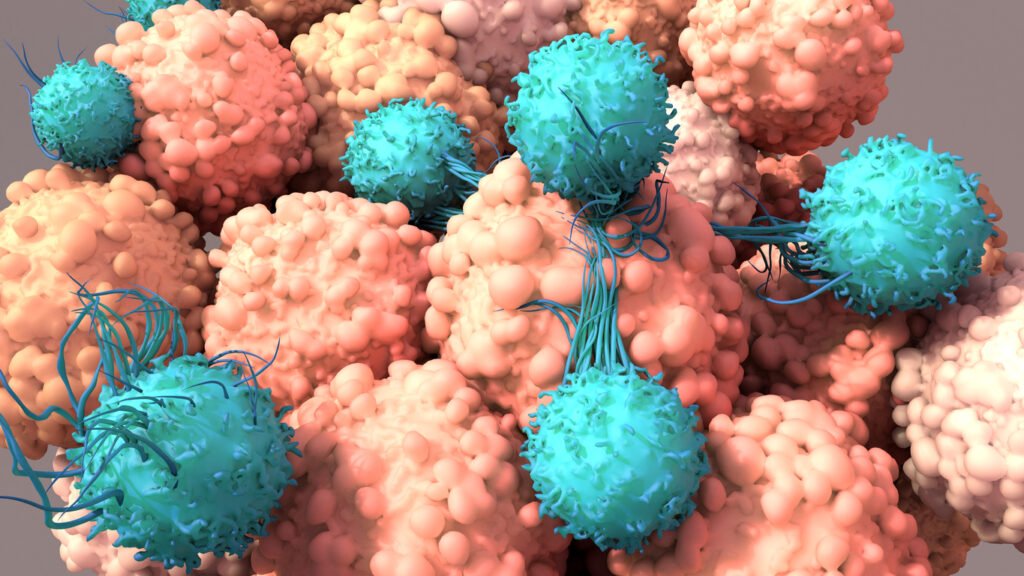
In a pre-clinical study, the researchers found a new treatment combination of Trametinib, a cancer drug that brings white blood cells to the site of the tumor and kills it, and Anti-PD-1, immunotherapy that blocks the signaling pathway.
It is important to note that is the combination of Trametinib treatment and immunotherapy that proved effective and not just one or the other.

“What we have done is that we have taken the drug that can inhibit the proliferation of the cells and suppress this immunosuppressive microenvironment. During this time, which is relatively short, we’ve been able to show that if you add immunotherapy then you can achieve what you want to achieve,” says Prof. Elkabets.
This sensitization happens because Trametinib inhibits the expansion of tumor cells. It also downregulates the immunosuppressive factor, meaning the cell decreases the quantity of a cellular component in order to respond to the foreign stimulus. This effect enables white blood cells that fight cancer to reach the tumor site, and kill the tumor cells efficiently, together with the Anti-PD1 immunotherapy.
The authors studied tumor-bearing mice and found in pre-clinical HNC models that treating them with this combination results in the disappearance of these tumors.
The “relatively short” time frame that Prof. Elkabets is referring to is around two weeks, he tells NoCamels.
Sign up for our free weekly newsletter
Subscribe“What is important is that you need to do it while the tumor is responding to the targeted therapy that we use, which in our case was Trametinib,” he explains, “If you wait a little bit longer, the tumor cells, again, organize the ecosystem and therefore is no longer active. There is an adaptation process that we want to interfere to achieve.”
The authors also showed for the first time in mice bearing HNC that the treatment should be given sequentially.
“It means that if you give only immunotherapy, it won’t work. If you give Trametinib and then after several weeks you start immunotherapy, it won’t work. You have a short, narrow window of time to apply this supplementation of immunotherapy,” he says.
When mice were treated with prolonged Trametinib treatment, tumors failed to respond to immunotherapy.
The major results are on multiple levels, he adds. “We’ve been able to show that if you apply the right treatment at the right time, you can achieve tumor elimination.”
Prof. Elkabets also says that the researchers were able to show that after the mice were cured, they actually developed immunization to the tumor.
“Even if it was injected again, the tumor did not grow,” he says.
This effective treatment was validated in four HNC cancer models, and most mice were cured with no recurrent disease. Together with Dr. Pierre Saintygn from Lyon the authors also validated some of the findings in HNC patients.
“Our unique ability to generate pre-clinical HNC models and to investigate new treatment and treatment combinations provides hope for HNC patients. We sincerely hope that oncologists will test this treatment combination in HNC patients, as improving immunotherapy efficacy is crucial for prolonging the survival of cancer patients,” Prof Elkabets said in a university statement.
The study was conducted by national and international groups from Soroka University Medical Center and Barzilai Medical Centers, Memorial Sloan Kettering, and Heidelberg Hospital.
Related posts

Israeli Medical Technologies That Could Change The World

Harnessing Our Own Bodies For Side Effect-Free Weight Loss

Missing Protein Could Unlock Treatment For Aggressive Lung Cancer



Facebook comments