To mark World Cancer Day, an international day to raise awareness of the disease, NoCamels is highlighting some recent medical developments in Israeli cancer research, treatment, and care – all from 2019-2020.
1. Israeli scientist’s research on curbing resistance to cancer treatment set to advance personalized care
Why does cancer therapy help some patients and not others? That is a question Israeli Professor Yuval Shaked of the Technion – Israel Institute of Technology in Haifa has been trying to answer with his latest medical research. Shaked recently published a study in “Nature Reviews Cancer,” a monthly review journal covering the field of oncology, that delved into how understanding and predicting individual host responses to cancer therapy can significantly improve care.
The initial cancer treatment phase can be often successful, but many patients are affected by the development of resistance, characterized by tumor relapse and/or spread, the Technion said in a statement.

“The majority of studies devoted to investigating the basis of resistance have focused on tumor-related changes that contribute to therapy resistance and tumor aggressiveness,” Shaked wrote. But over the past decade, the diverse roles of various host cells in promoting therapy resistance have become better understood. The current understanding is that cancer therapy can induce local and systemic responses in the patient’s body, and these actually support the resurgence of cancer and its progression.
“Current modern immunotherapy has revolutionized cancer care,” Shaked said in a Technion statement. “However, despite considerable advances in cancer treatment, most patients do not respond to therapy at all or from a particular stage. Without the ability to predict the effectiveness of treatment, many suffer from disease recurrence or spread, which sometimes erupts with even greater violence.”
“Over the years, many have investigated and are still investigating the effect of therapy on the tumor itself, but few have analyzed the effect of the therapy on the patient,” he pointed out.
This shift in focus can produce better care and help advance personalized and precision medicine, he indicated.
“We are not saying that existing treatments are not good,” he emphasized in the statement. “They just aren’t suitable for everyone. Each treatment triggers a host response, and when this response exceeds the therapy effect, we receive ineffective treatment. For the therapy to be effective at the specific host level, it is important to predict the same counter-response and try to block it. This is how we will gain much more effective therapy.”
Shaked is the head of the Technion Integrated Cancer Center and the chief scientific advisor of OncoHost – a company he founded that uses response profiling to improve personalized cancer therapy.
OncoHost recently opened a new state-of-the-art laboratory in Binyamina for this very research and has already begun clinical trials in Israel. The company is in talks to start trials in Europe and the US, Shaked said,
It was recently awarded a $1 million grant as part of the Binational Industrial Research and Development (BIRD) Foundation to advance its research.
“For immunotherapy, one of the most important effective approaches today in the field of cancer, only some 20-30 percent of patients today respond. Through blood testing, we can predict the outcome of patients treated with immunotherapy and continue such treatment only in patients in whom treatment is expected to be effective,” he said.
“Based on the present study, in the future, we may offer combined therapies to increase the effectiveness of treatment or allow patients who are currently unresponsive to immunotherapy drugs to respond to them. This is a huge revolution that we must advance not only in research but also in the commercialization of research into actual therapies. Only then can we contribute to saving lives,” he added.
2. Israeli medical tech startup delivers promising clinical trial results with new cancer therapy
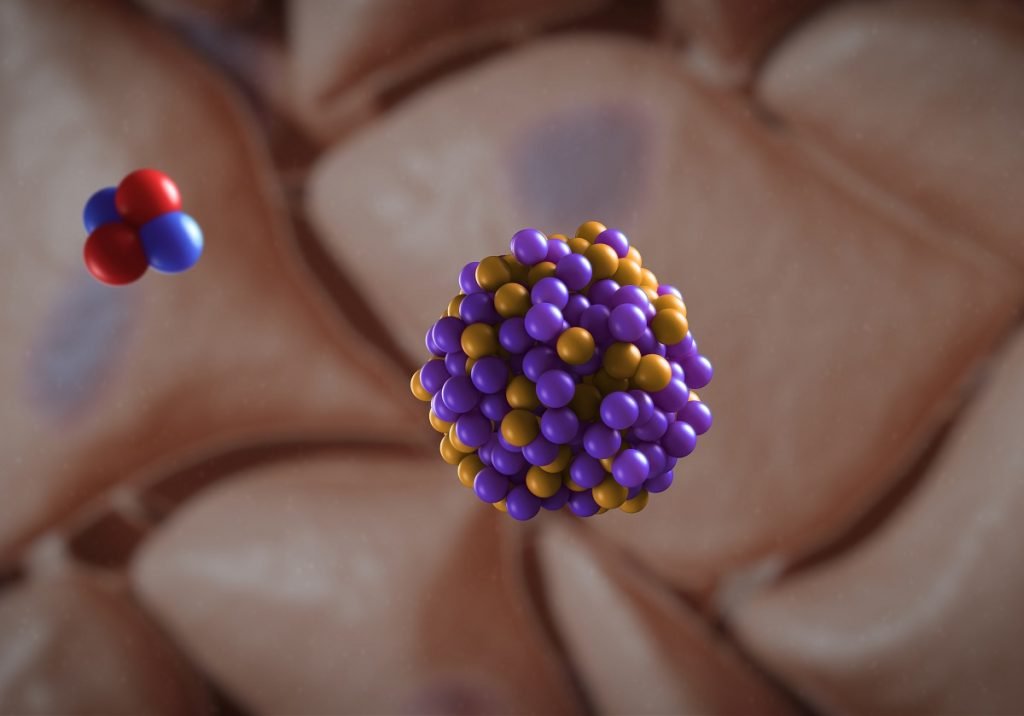
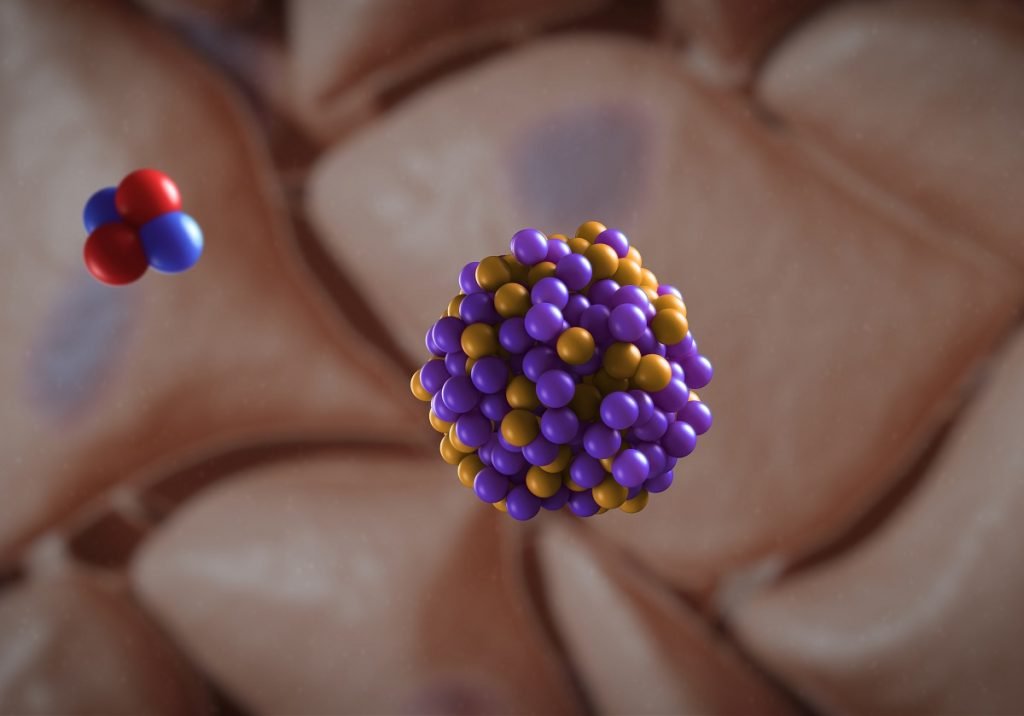
Israel’s Alpha Tau Medical, an Israeli medical technology company that developed breakthrough radiation cancer therapy, announced late last year that initial results of a preclinical trial have proved very promising.
Alpha Tau Medical was founded in 2016 to focus on R&D and commercialization of its breakthrough cancer treatment, Alpha DaRT (Dіffusіng Alpha-emіtters Radіatіon Therapy). The technology, initially developed in 2003 by Professors Itzhak Kelson and Yona Keisari at Tel Aviv University, delivers high-precision alpha radiation that is released when radioactive substances decay inside the tumor, killing cancer cells while sparing the surrounding healthy tissue.
The first clinical trial of the treatment was conducted in Israel and Italy starting in 2018. The trial was designed to establish the safety, feasibility, and efficacy of the company’s Alpha DaRT technology for patients with squamous cell carcinoma of the skin and head and neck area.
The results, published in the International Journal of Radiation Oncology, Biology, and Physics, showed nearly 78.6 percent of 28 patients received a complete tumor response rate. That means the patients all responded to the alpha radiation treatment in some way.
“Overall, these impressive outcomes serve as an excellent basis for future trials in other tumor types,” said the principal investigator of the trial Prof. Aron Popovtzer, MD, from Rabin Medical Center in Israel. The Italian arm of the trial was led by Dr. Salvatore Roberto Bellia from the IRST (Istituto Scientifico Romagnolo per lo Studio e la Cura dei Tumori).
Future clinical trials will also investigate Alpha DaRT in other oncology indications, as a monotherapy or in combination with various systemic therapies.
3. Israeli scientists find a molecule that triggers self-destruction of pancreatic cells
Late last year, Israeli scientists said a new study they conducted showed that a small molecule called PJ34 triggered the self-destruction of human pancreatic cancer cells in mice.
Sign up for our free weekly newsletter
SubscribeAccording to the research, published in the peer-reviewed open-access biomedical journal Oncotarget, the administration of the molecule reduced the number of cancer cells in developed tumors by up to 90 percent in 30 days.
The study was led by Professor Malka Cohen-Armon and her team at Tel Aviv University’s Sackler Faculty of Medicine, in collaboration with Dr. Talia Golan and her team at the Cancer Research Center at Sheba Medical Center, and conducted with transplantations of human pancreatic cancer cells into immunocompromised mice, or xenografts.
Professor Cohen-Armon indicated that the mechanism, tested in parallel studies, acted efficiently in additional types of cancer, eradicating a variety of resistant cancer cells (breast, lung, brain, and ovarian cancer) including types resistant to current therapies.
PJ34 is being tested in pre-clinical trials according to FDA regulations before clinical trials on larger animals and then humans begin, Tel Aviv University said in a statement at the time.
Dr. Golan is a lead researcher at the Pancreas Cancer Olaparib Ongoing (POLO) Clinical Trial at the Sheba Medical Center.
4. Israeli oncologist offers hope with a new treatment for some pancreatic cancer patients
This past summer, NoCamels reported on Dr. Golan’s work on a drug regimen that proved promising for some pancreatic cancer patients, specifically those with advanced stages of the disease as well as a BRCA 1 or 2 germline mutation.

BRCA1 & 2 are tumor suppressor genes, meaning that those with the deleterious mutation have a higher lifetime risk of developing cancer. The gene is predominantly linked to breast and ovarian cancer, but several studies name pancreatic cancer as the third most common cancer associated with these mutations.
Among patients with pancreatic cancer, only four to seven percent have this gene variation, so Dr. Golan’s clinical trial team looked for participants from across the world.
Dr. Golan tested the effectiveness of a drug regimen that featured a PARP inhibitor called Lynparza, the trade name for the biological agent olaparib. The drug blocks the production of Poly ADP-ribose Polymerase (PARP), a protein that repairs DNA in tumor cells.
Her study, published in the New England Journal of Medicine, explained: “PARP inhibitors cause an accumulation of DNA damage and tumor-cell death. The PARP inhibitor olaparib has been shown to have clinical efficacy in patients with a germline BRCA mutation and ovarian or breast cancer.”
The results of the Phase III randomized, double-blind study with a placebo control group showed that, in essence, the drug treatment regimen stalls the progression of the disease. Of the 3,315 patients who underwent screening, 154 fit the study criteria to be assigned to trial intervention, thus 92 received the treatment and 62 received the placebo.
“The median progression-free survival was significantly longer in the olaparib group than in the placebo group (7.4 months vs. 3.8 months),” the study detailed.
5. Could a simple blood test screen for lung cancer?
Israeli and British scientists published a new study in October that showed that a simple blood test that relies on a “DNA repair score” proved effective for lung cancer screening.
The study was led by Professor Zvi Livneh and Dr. Tamar Paz-Elizur, both members of the Weizmann Institute Department of Biomolecular Sciences, alongside Professor Sir Bruce Ponder of the University of Cambridge and Professor Robert Rintoul from Royal Papworth Hospital and Cambridge.
Titled “DNA-Repair Biomarker for Lung Cancer Risk and its Correlation with Airway Cells Gene Expression” and published in the peer-reviewed journal the National Cancer Institute-Cancer Spectrum (JNCI-CS), the scientists’ study found that patients’ “DNA repair scores” – a summation of the activity of three DNA repair enzymes (OGG1, MPG and APE1) through which cells are known to respond to genetic damage – can “significantly improve current lung cancer risk prediction, assisting prevention and early detection.”
The study involved 150 British patients with non-small-cell lung cancer and a control group of 143 healthy volunteers. The scientists calculated each participant’s DNA repair score “based on blood activity levels of three enzymes known to respond to DNA damage,” the Weizmann Institute said in a statement.
They found that the DNA repair score of those with lung cancer was lower than the control group across the board, “establishing this enzymatic activity as a robust biomarker for lung cancer risk – independent of smoking.”
The results, the Weizmann Institute said, validated a previous study published in 2014 by Professor Livneh that examined DNA repair scores in an Israeli population, “showing that the new approach could potentially be implemented to promote more effective lung cancer screening worldwide.”
Reliance on age and smoking status as the two main risk factors “isn’t enough, as preventative screening in this selected population misses most lung tumors,” the Israeli and British scientists wrote in their paper. “Moreover, individuals who are not obvious candidates for screening remain unaware of the danger they may face – leading to delayed treatment and poorer prognosis,” they went on.
Related posts

Israeli Medical Technologies That Could Change The World

Harnessing Our Own Bodies For Side Effect-Free Weight Loss

Missing Protein Could Unlock Treatment For Aggressive Lung Cancer



Facebook comments