An Israeli scientist has been awarded a US patent for his innovative vaccine design for the corona family of viruses, and is on track to develop a vaccine for the novel coronavirus.
Tel Aviv University said in a statement this week that Professor Jonathan Gershoni of the School of Molecular Cell Biology and Biotechnology at TAU’s George S. Wise Faculty of Life Sciences was awarded a patent by the US Patent and Trademark Office (USPTO) for a vaccine that targets the Achilles’ heel of coronaviruses, that is their Receptor Binding Motif (RBM), “a critical structure that enables the virus to bind to and infect a target cell.”
In the case of the novel coronavirus, the RBM is part of its “spike” protein, which is the major viral surface protein that it uses to direct how the virus engages and interacts with cells of the body and to bind to a receptor “like a key that has to fit into a keyhole,” Prof. Gershoni tells NoCamels.
According to Prof. Gershoni, the vaccine would reconstruct the coronavirus’s RBM. After the spike protein binds to the human cell receptor, the viral membrane fuses with the human cell membrane, allowing the genome of the virus to enter human cells and begin infection.
The spike protein for the novel coronavirus is large, containing about 1,200 amino acids. Some researchers have limited their research to a region of the spike known as the receptor-binding domain (RBD) that comprises some 200 amino acids. However, the problem is that these relatively large areas have a variety of targets, and the immune system produces antibodies for all of them indiscriminately — reducing the effectiveness of a potential vaccine.
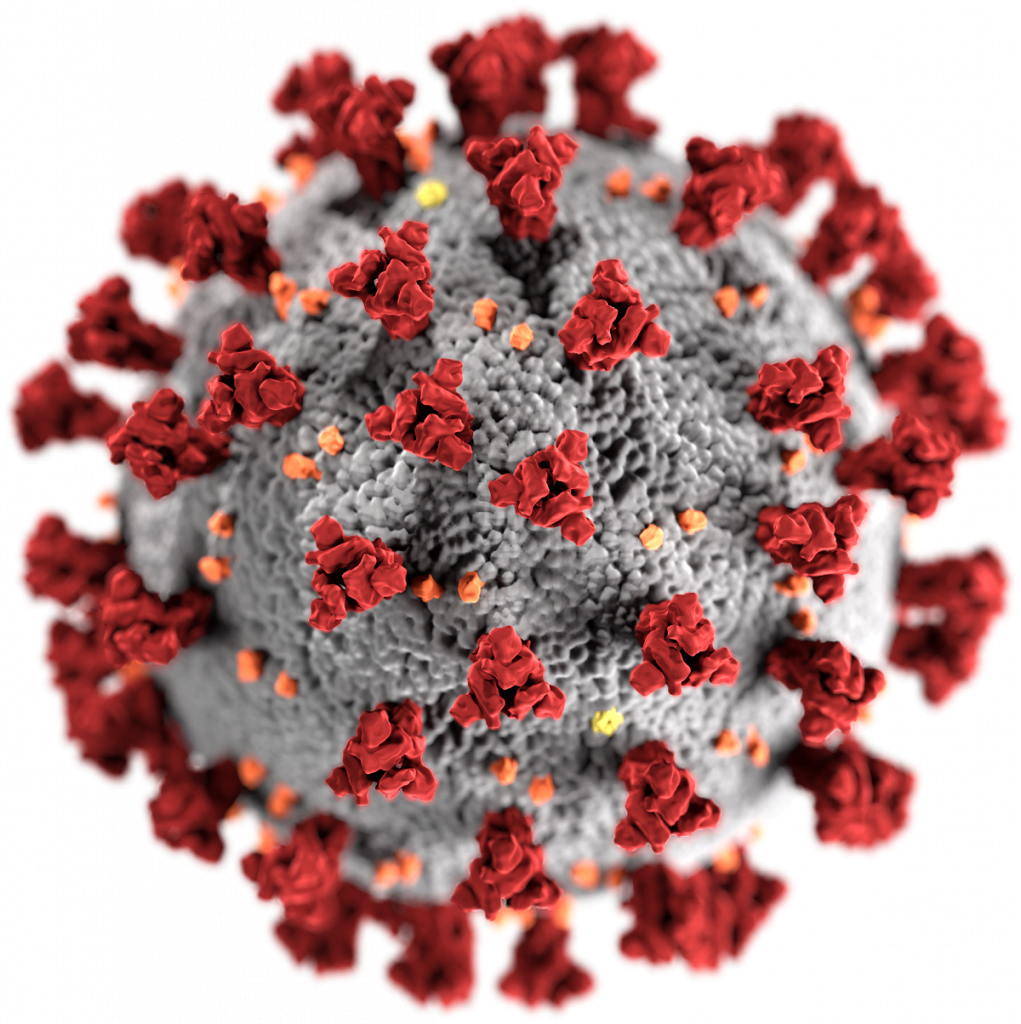
Gershoni and his team, who have been working on coronaviruses since 2004, around the time of the first SARS (severe acute respiratory syndrome) outbreak caused by SARS-CoV, are already ahead of the game. Over the course of four to five years, the team has already identified the 50 amino acids that make up the RBM, the highly complex three-dimensional structure this critical component of the virus.
“We have been using tricks of molecular biology to identify weak spots in hopes of outwitting the virus,” he explains. “We hope to isolate the weak spot [in this particular virus.] This is how we can reconstitute it.”
Functionally reconstituting such a structure, while challenging, would be an extremely effective basis of a vaccine, says Prof. Gershoni.

“We have been working on coronaviruses for the last 15 years, developing a method of reconstructing and reconstituting the RBM feature of the spike protein in SARS CoV and subsequently in MERS CoV,” he said in a university statement.
“The smaller the target and the focus of the attack, the greater the effectiveness of the vaccine,” he adds. “The virus takes far-reaching measures to hide its RBM from the human immune system, but the best way to ‘win the war’ is to develop a vaccine that specifically targets the virus’s RBM.”
The scientists began working with the genome of the novel coronavirus, known as SARS-CoV2 (which causes the COVID-19 disease) in early January.
Prof. Gershoni and his team completed their initial steps toward reconstituting the new SARS CoV2’s RBM, the university said. Its use as a basis for a new vaccine is covered by an additional pending patent application, filed by TAU’s technology transfer arm Ramot to the USPTO.
“Now that we have received serum samples we should be able to isolate RBM-based vaccine candidates in the next month or two,” Prof. Gershoni said. “The discovery and production of a functional RBM for the new coronavirus is fundamental and critical for the production of the vaccine we propose.”
Prof, Gershoni said they expect to provide a “blueprint” of the reconstituted RBM very soon.
Sign up for our free weekly newsletter
Subscribe“Once we have a solution, we want to partner with a pharmaceutical company,” he tells NoCamels, “Within the next two or three months, we will be in a position to know whether we have been successful or not, hopefully the latter. Then we should be able to effectively partner with the industry to produce an effective vaccine. “
The vaccine could be ready for use within a year to a year and a half, he indicated.
“Our successful isolation and reconstitution of such a functional RBM will allow the industry to incorporate it into a vaccine, which will be produced by a pharmaceutical company. Development of such an RBM-based vaccine should take months and then would need to be tested in Phase 1, 2 and 3 clinical trials which would then take up to a year,” he said.
The vaccine would also need to go through the usual process of getting FDA approval, Gershoni said.
COVID-19 has killed over 170,000 people across the globe and nearly three million have been infected.
Israeli vaccine development for coronavirus
A number of Israeli scientific teams are currently working to develop a vaccine for COVID-19.
Earlier this month, the Israel Institute for Biological Research (IIBR) reported “significant progress” toward a vaccine. A source familiar with the institute’s activities told Reuters and other media outlets that trials were already underway on rodents, without specifying which type.
Israel’s Migal Research Institute in the northern Israeli town of Kiryat Shmona is also working on a vaccine for COVID-19. In early March, Migal scientists said that they have successfully developed a new vaccine for a deadly virus affecting poultry and are now working to adapt the vaccine for humans.
Rehovot-based company Kamada, a commercial-stage plasma-derived biopharmaceutical company, announced a few weeks ago that it was developing a “passive vaccine” for the coronavirus as a potential treatment for severely ill patients.
The company specializes in the extraction and purification of proteins from human plasma to produce immune globulins. “The plasma-derived Anti-Corona (COVID-19) IgG product is expected to be produced from plasma derived from donors recovered from the virus, which is anticipated to include antibodies to the novel coronavirus,” Kamada said.
Global efforts toward a vaccine and treatment
Over 70 vaccine candidates or treatment for the coronavirus are in the works, according to an updated list by the World Health Organization. China, where the outbreak began in December, quickly shared the genetic material sequence of the coronavirus allowing research groups to begin studies.
US company Moderna was first out the gate, having announced in February that it shipped out an experimental vaccine for testing at the National Institute of Allergy and Infectious Diseases (NIAID). Clinical trials on humans have begun.
California-based biotech firm Gilead Sciences is currently in a Phase III clinical trial to evaluate the safety and efficacy of its novel antiviral drug Remdesivir, developed originally for Ebola, in adults diagnosed with COVID-19. These trials build on additional research including two clinical trials in China’s Hubei province led by the China-Japan Friendship Hospital, and a clinical trial in the US-led by NIAID. Initial results have shown promise.
Related posts

Israeli Medical Technologies That Could Change The World

Harnessing Our Own Bodies For Side Effect-Free Weight Loss

Missing Protein Could Unlock Treatment For Aggressive Lung Cancer





Facebook comments