This article was first published on The Times of Israel and was re-posted with permission.
The worst form of brain cancer, glioblastoma multiforme (GBM), is considered largely incurable by doctors. Victims generally die within a year and a half of being diagnosed with the tumors. It’s such a devastating disease that the National Academy of Sciences calls it “the Terminator.” But an innovative nanotech-based “end-run” around cancer cells by Tel Aviv University researchers could provide doctors with a new way to treat – or even cure – GBM and other malignant killer cancers.
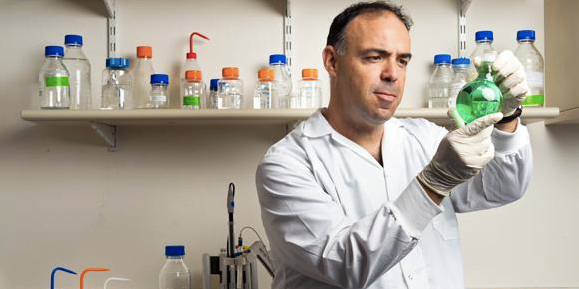
The technique, developed by Prof. Dan Peer of TAU’s Department of Department of Cell Research and Immunology and Scientific Director of TAU’s Center for NanoMedicine, has proven itself in the past: It’s based on the “cancer bullet” system Peer and other TAU researchers developed that delivers chemotherapy directly to cancer cells, using bioadhesive liposomes (BALs), consisting of regular liposomes reduced to nano-sized particles that attach themselves to the cancerous cells. Peer and Prof. Rimona Margalit, with whom he developed the method, have published several studies showing its effectiveness.
That research was done on ovarian cancer tumors, and it proved to be effective – but that wasn’t the case when it came to GBM, which is far less responsive to chemotherapy. Prof. Zvi R. Cohen, Director of the Neurosurgical Oncology Unit and Vice Chair at the Neurosurgical Department at Sheba Medical Center at Tel Hashomer Hospital in central Israel, contacted Peer to discuss whether anything could be done for individuals suffering from the aggressive and fatal form of brain cancer.
SEE ALSO: Cancer Breakthrough: Israeli Researchers Discover Cancer Suppressing Proteins
“I was approached by a neurosurgeon insistent on finding a solution, any solution, to a desperate situation,” said Peer. “Their patients were dying on them, fast, and they had virtually no weapons in their arsenal. Prof. Zvi Cohen heard about my earlier nanoscale research and suggested using it as a basis for a novel mechanism with which to treat gliomas,” the cancers that originate in glial cells in the spine or brain, of which GBM is the most devastating.
Cohen had acted as the primary investigator in several glioma clinical trials over the last decade, in which new treatments were delivered surgically into gliomas or into the surrounding tissues following tumor removal.
To continue reading this article on the TOI site, click here.
Related posts

Israeli Medical Technologies That Could Change The World

Harnessing Our Own Bodies For Side Effect-Free Weight Loss

Missing Protein Could Unlock Treatment For Aggressive Lung Cancer




Facebook comments