An Israeli startup is developing a new protein-based cancer treatment that it says has the potential to address one of the most important oncology targets. ExoProTher says its therapy solely affects the mutated cells that form tumors, and, unlike other treatments, does not affect healthy cells.
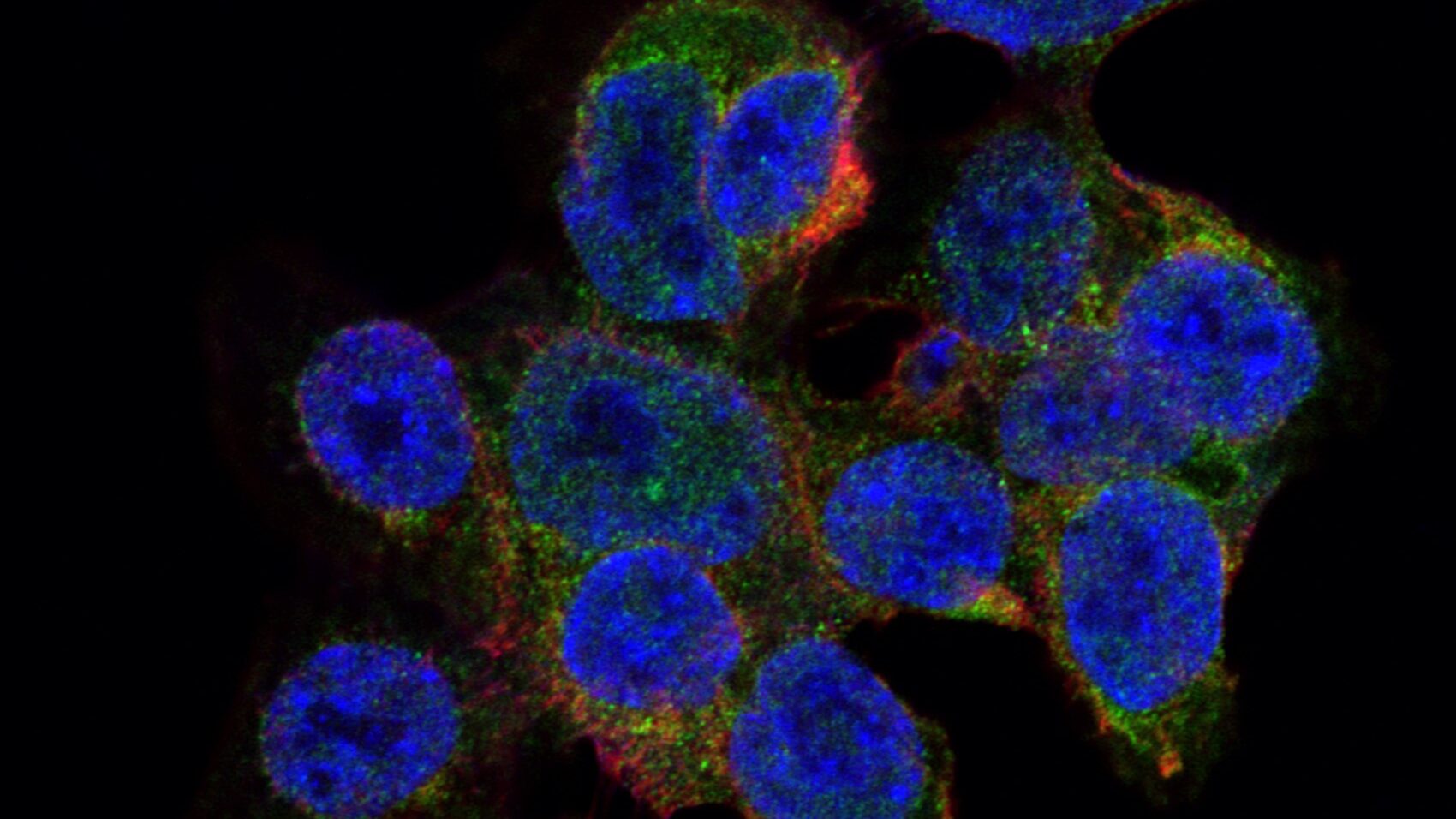
Now being tested in the preclinical stage, the drug uses the p53 protein, which suppresses tumors. The p53 molecules bind to damaged DNA and tell cells with irreparable DNA damage to go into apoptosis (cell death). This prevents cells with damaged DNA from grouping together and forming tumors.
Israeli scientists Lana Volokh and Alex Tendler co-founded the startup (whose name derives from EXOsome PROtein THERapy) in 2017, to develop a drug using protein from chicken cells.
They say there are no apparent side effects from the treatment and claim it could even replace chemotherapy, which is one of the most common cancer therapies. More than half of oncology patients worldwide were treated with chemo in 2018.
Chemotherapy targets cancer cells to stop them from reproducing but healthy cells are also damaged during the process as the drugs cannot distinguish between them. This causes multiple negative side effects such as hair loss, intense nausea, anemia, and damage to memory and concentration.
Tumor Terminator
P53 was first discovered in 1979 when scientists noticed the protein sticking to infected cells and signaling antibodies to fight infection. In 1989, the gene that produces the protein was determined to be a tumor suppressant.
Dr. Tendler claims nobody has succeeded in developing a therapy based on the p53 protein delivery until now.
“Twenty years ago, it was discovered that when the healthy protein interacts with the p53 mutated cells, the mutated proteins prevent the healthy ones from working,” he tells NoCamels.
“We solve the biggest problem by the usage of protein from other species. We use the protein from chicken cells, which is proven to be able to perform its function in human cells, but not to the point where the mutated human proteins can prevent it from working,” he said.
“We solved this problem by usage of xenogeneic protein (protein originating from other, non-human, species). We use the protein of chicken origin. We successfully demonstrated that chicken p53 protein is able to perform its anti-cancer function in human cells while it is not inhibited by mutated p53 protein.”

Dr. Volokh says nobody has previously considered using chicken protein.
“Our approach is distinct from all of the current companies in the active substance, how we deliver the protein, and how the whole product is going to look,” she says.
“Chicken protein is similar enough to function in human cells but not to the point where the mutated protein molecules can prevent them from working,” Dr. Tendler explains.
The two scientists decided to explore p53 protein as cancer treatment when they realized that even though the cornea (the outer layer of the eye) is continually exposed to UV radiation from the sun, it is extremely rare to see that part of the body stricken with cancer.
“It turns out that there is a huge amount of p53 protein in the cornea, already packed in the nanovesicles released by corneal cells,” says Dr. Tendler.
Nanovesicles are tiny sacs particles that transport materials in and out of cells.
“Those vesicles are released by corneal cells into extracellular spaces, and circulate throughout the cornea. Those vesicles can even be found in tears. When there is a mutated p53 cell, it instantly gets healthy protein from the neighboring cells. So this is a local defense mechanism against cancer.”
Sign up for our free weekly newsletter
Subscribe
In fact, says Dr. Tendler, 60 percent of cancers are associated with mutation of the gene encoding the p53 protein.
By delivering p53 proteins through extracellular vesicles, the healthy proteins can drive the mutated cells into apoptosis and restore the body’s natural defense mechanisms against cancer.
Based in Haifa, ExoProTher is currently funded by Israeli investing giants Israel Biotech Fund and Peregrine Ventures.
In their preclinical trials, Drs. Tendler and Volokh say they were able to significantly prolong the lives of mice with tumors and substantially reduce metastasis (the spread of cancer cells throughout the body). They were also able to show that the drug has no toxic side effects.
Furthermore, they say, their drug will be suitable for a range of cancers.
“We have screened a lot of different cancers,” says Dr. Tendler. “We see the ability to affect and potential to cure very different cancers. Colon cancer, brain cancer, lung cancer, ovarian cancer.”
Cost Effective
Dr. Volokh also believes ExoProTher’s protein therapy can drastically reduce the cost of cancer treatment, highlighting the price of therapies that are tailored to the patient’s own individual genetic makeup.
“There are many therapies today where blood is derived from the patient and the doctors engineer the drug substance to match that particular profile of that patient, which means that the drug is not applicable to anyone else,” she says.
“That’s what makes certain therapies so expensive. But in our case, the drug will be an off-the-shelf product ready for administration, applicable to almost every type of cancer where p53 function is affected. This fact will allow large-scale manufacturing of our substance and make the therapy affordable. The vesicles can be administered through standard injection and also through inhalation.”
A 2019 study by the Mesothelioma Center found that over 60 percent of cancer patients in the US reported financial struggles following their diagnosis. In fact, the American Association for Cancer Research says that the annual cost of cancer care in the US will likely reach around $246 billion by 2030, a 34 percent rise since 2015.

Tendler and Volokh say their protein therapy could initially be used alongside other treatments, including chemotherapy, and eventually even replace them.
“We expect synergy between chemotherapy and our treatment,” Dr. Tendler says.
“Our drug will be able to sensitize the tumors to chemotherapy and reduce the amount of chemo drugs that the patients will need, thus reducing chemotherapy’s side effects. This will probably be the first step before it becomes a standalone drug.”
Dr. Volokh says their goals for the rest of 2023 are to continue lab trials and ensure higher yield and reproducibility rates for the drug substance, which are important for mass manufacturing.
“Actually, Israel has a very strong leadership position in all that is about the p53 protein. Israel has a very rich history of discovery and characterization of p53-related mechanisms. Our ambition is to develop a p53 targeting drug here in Israel and make p53 an actionable clinical target. That’s our vision,” says Dr. Tendler.
“There is not a single drug yet like this. It has the potential to make a huge impact.”
Related posts

Israeli Medical Technologies That Could Change The World

Harnessing Our Own Bodies For Side Effect-Free Weight Loss





Facebook comments