A recently released Tel Aviv University (TAU) study reported improvements in memory capacity, attention, and information processing speed in Alzheimer’s disease patients and those with dementia through the use of hyperbaric oxygen therapy (HBOT).
The team of investigators remarked that this was the first time that non-drug therapy has been proven effective in preventing the core biological processes responsible for the development of Alzheimer’s disease.
The study was conducted under the leadership of a team of TAU investigators including Professor Shai Efrati, Professor Uri Ashery, Dr. Ronit Shapira, Dr. Pablo Blinder, and Dr. Amir Hadanny. All of them are members of TAU’s Sagol School of Neuroscience and the faculties of Life Sciences and Medicine, as well as associates of the Shamir Medical Center. The findings of the breakthrough study were published in the journal Aging.

In an interview with NoCamels, Professor Uri Ashery, who is an associate of the TAU’s Sagol School of Neuroscience and the faculties of Life Sciences and Medicine, as well as associates of the Shamir Medical Center reflected at greater length on the significance of the study’s findings.
“Hyperbaric oxygen treatment has been used for decades already,” Prof. Ashery said. “Most people would recognize hyperbaric treatment to treat divers following rapid oxygen decompression. Patients enter a chamber of two atmospheric pressure with an added 100 percent oxygen. The idea is to increase the solubility of oxygen in the blood by a factor of 10. We’ve seen the effect of this most recently in the treatment of COVID-19 patients; without it the disease there is 95-98 percent oxygenation of the blood. We know that if blood oxygenation drops below 92 percent then the patient is in trouble.”
SEE ALSO: Experimental Alzheimer’s Drug May Help Kids With Autism, Says Leading Israeli Neuroscientist
“In addition to treating the bends, or people with wounds who are not healing, HBOT is also used to treat diabetic ulcers. It is only relatively recently that it has been used to treat brain disorders,” Prof. Ashery adds. “It has been shown to help patients with stroke – many years after stroke happened – and we are looking at the possibility of treatment to improve cognition.”
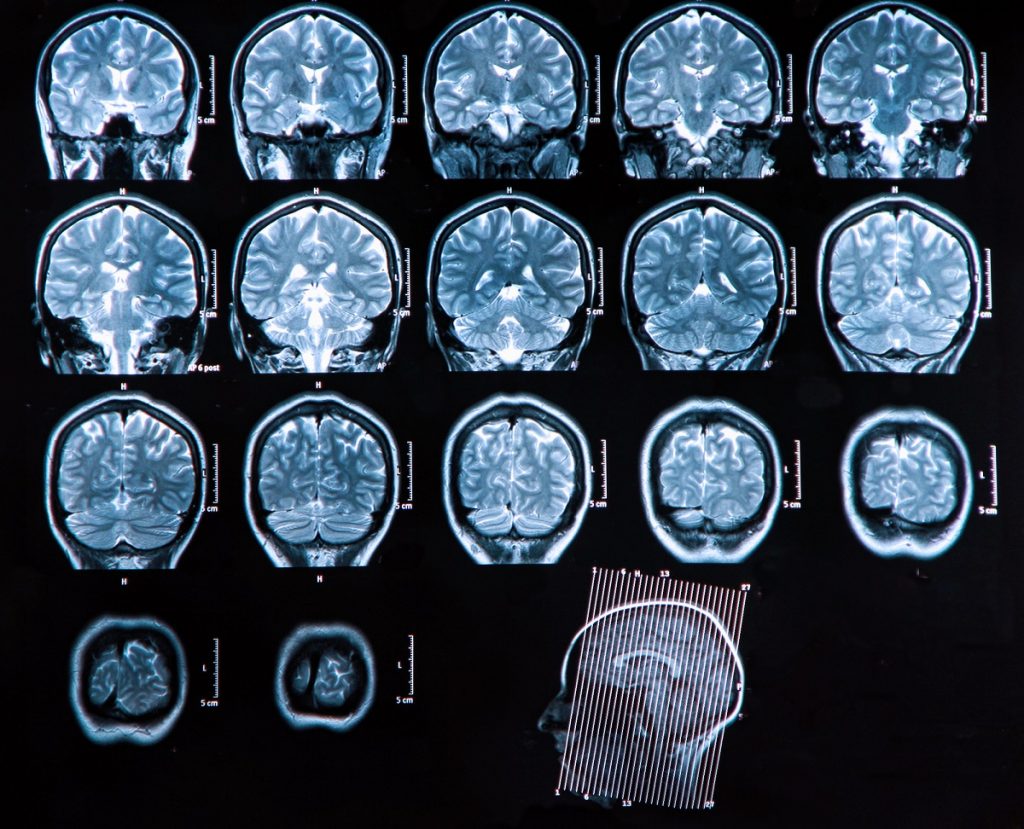
The first stage of the study was carried out on an animal model – using mice – in the course of which it was proven conclusively through examination of brain tissues that a certain therapeutic protocol brings about an improvement in vascular function and the creation of new blood vessels. It also prevents the deposit of new amyloid plaques on the brain cells and even leads to the removal of existing amyloid plaque deposits. Deposits of such non-soluble amyloid proteins in the brain are connected with severe degenerative conditions such as Alzheimer’s disease.
Sign up for our free weekly newsletter
Subscribe
“We treated them for a month for one hour per day,” Prof. Ashery recalls. “We found many improvements, including in the blood supply; and with better blood flow we saw that the treatment prevented vascular constriction. There was also an increased ability to learn.”
The second part of the study was that a clinician had a group of patients with reduced cognitive abilities “but had not yet been diagnosed,” Prof. Ashery explains. “They exposed patients for 60 daily treatments for a period of three months – for approximately one to one-and-a-half hours per day. We identified that they got significant improvement in cognitive abilities, between 15-16 percent in memory, a six-percent improvement in attention and a more than 10-percent-increase in blood flow in the brain.”
The researchers tested several memory areas, in particular the improvements in short-term and working memory. Prof. Ashery notes that the memory tests are performed with a computer-based program, which can investigate many different types of memory and provides scores without creating any experimental bias.

Prof. Ashery admitted that at this stage of the study it is difficult to conclude whether there is – like in the case of mice – a cumulative effect of improvement. “We have not yet followed the patients for enough time, although there are longer studies that have followed patients for some three months. However, it seems likely that if this treatment works as we think it does, it would need to be maintained. It is something that we will have to examine.”
It seems that for patients who have suffered a stroke, HBOT holds for several months. “For a neurodegenerative disease, we will almost certainly have to maintain the treatment to witness the kinds of improvements that seem to be possible.”
Viable treatments for Alzheimer’s disease are notoriously slow in development, although Prof. Ashery did provide a message of hope. “While it is true that there is currently no cure for Alzheimer’s disease, we hope that by using a treatment that has been shown to be working well for many other illnesses, it will allow us to move to the next phase of implementing treatments without the need for drugs. It is also true that HBOT seems more useful for the early stages of cognitive decline and our study does indeed show its efficacy.
Related posts

Editors’ & Readers’ Choice: 10 Favorite NoCamels Articles

Forward Facing: What Does The Future Hold For Israeli High-Tech?

Impact Innovation: Israeli Startups That Could Shape Our Future



Facebook comments