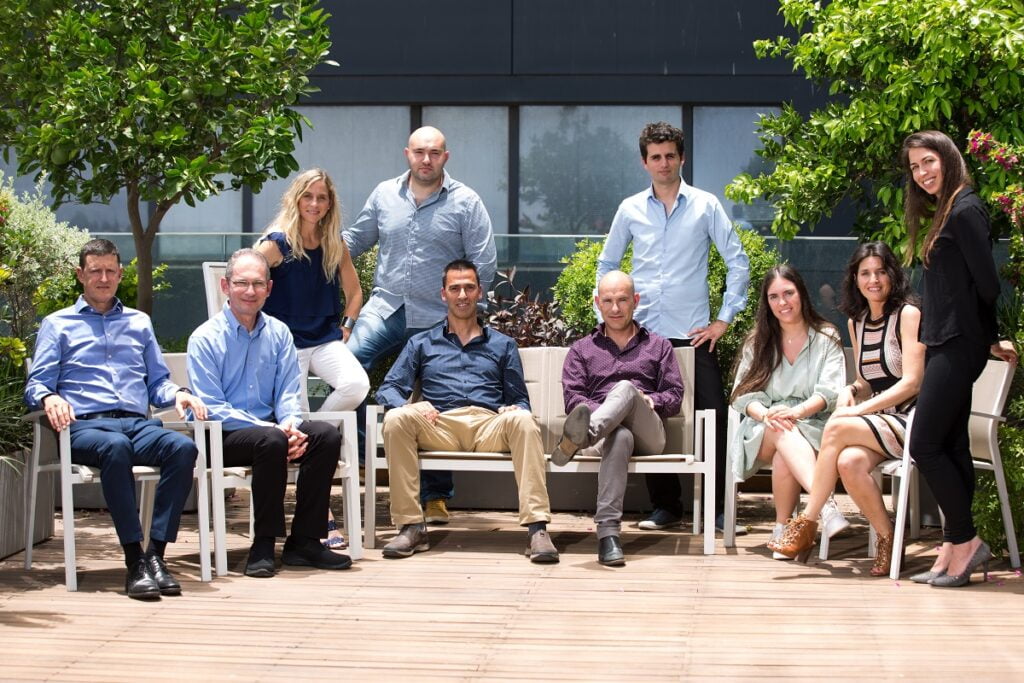
During the start of the COVID-19 pandemic, the ophthalmic community was forced to halt all harvesting of tissues for eye procedures, impacting expected surgeries such as corneal transplants (keratoplasty) and for glaucoma. As a result, many people suffered from a lack of access to treatment or corneal lenses, according to Dr. Gilad Litvin, co-founder and chief medical officer at CorNeat Vision, an Israeli medical device startup founded in 2015 that develops synthetic ophthalmic implants.
As corneal tissues are often taken from donor patients in the morgue or at the bedside shortly after the patient passes away, many ophthalmologists did not want to risk contracting the virus or take a corneal sample that would test positive for COVID-19, Dr. Litvin describes.
As such, the Raanana-based CorNeat Vision has been touting its ophthalmic biomimetic, or synthetic, implants. “We believe that a synthetic substitute would alleviate many shortcomings [of reconstructive surgery] and would give a solution that will be much safer, especially in these COVID-19 days; you have harvested tissue you don’t know who’s sick and is completely synthetic and sterile,” Litvin tells NoCamels.
SEE ALSO: AEYE Health’s Simple Eye Scan To Diagnose, Prevent Avoidable Blindness
CorNeat offers a few innovative solutions including the CorNeat KPro, an artificial cornea, and the CorNeat EverPatch, an artificial connective tissue substitute.
The CorNeat KPro implant is designed to replace deformed, scarred or opacified corneas and is expected to fully rehabilitate the vision of corneally blind patients, the company says. The CorNeat KPro’s lens integrates with resident ocular tissue using a patented synthetic non-degradable nano-fabric placed under the conjunctiva (the tissue that lines the inside of the eyelid). Current biological solutions are either sutured to or become integrated with native corneal tissue, which lacks blood vessels and heals poorly, Dr. Litvin explains.
“The holistic statement that we have as a company is to attempt to give back sight to people who are blind, to cure ophthalmic disease in that fashion, [and] try to bring more quality of life, greater equality and sustainability to our societies worldwide,” he tells NoCamels.
“Some of the indications that cause blindness, specifically corneal blindness. are more prevalent in less privileged areas, and it’s our mission to make profits but also to support these areas in the world as well,” Litvin adds.
CorNeat’s patented implants utilize advanced cell technology and nanoscale chemical engineering to mimic the structure and function of cellular and subcellular structures, which stimulates cellular growth and facilitates complete integration with surrounding tissue.

“The challenge [of this technology] is to embed this artificial material within our own tissue, and we know that any foreign body that goes into our body, usually the body tries to push it out or encapsulate it,” Litvin says.
“We use a chemical engineering technology called electrospinning, and with this technology, you create a very high voltage electrical field, and you manufacture your polymeric fibers through this very strong electrical field. This allows you to calibrate the thickness of the fibers to a very small scale, nanometric and micrometric scale, and this scale imitates our own tissue microanatomy,” he explains.
CorNeat KPro snaps into the patient’s trephined cornea and is then sutured to the eye using three non-degradable sutures, which reduces risk and minimizes the time the eye is trephined and open to less than one minute. The KPro lens enables post-operative ophthalmic examinations and subsequent surgeries like cataract surgery. Additionally, the KPro cannot carry any infectious agent including COVID-19.
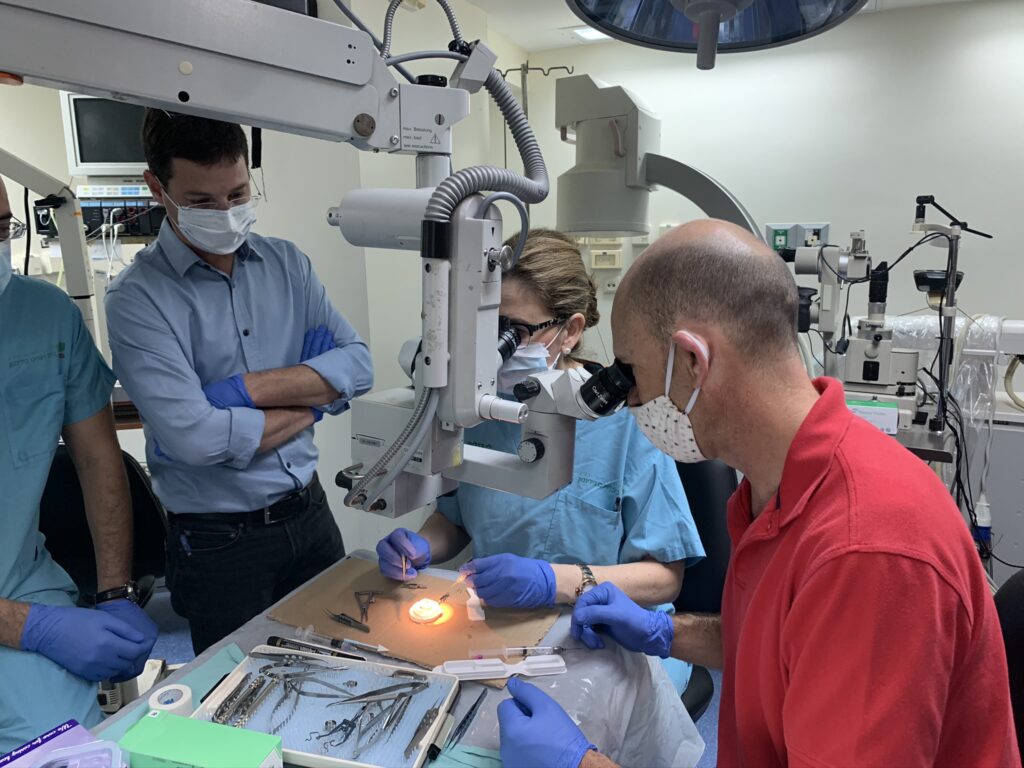
“We wanted to create a device that doesn’t need any tissue, if you could have a completely synthetic alternative to the human donor tissue,” Litvin says. “The second target was to create a procedure that would be simple to perform, something that would be simple to teach and would create a feeling of self-confidence in our surgeons when they attempt to perform this for the first time and later on.”
CorNeat’s synthetic cornea approved for 1st human implantation
In July, CorNeat announced that its KPro has received approval to begin a clinical trial at Beilinson Hospital in Petah Tikva. The trial was approved by Israel’s Ministry of Health and will include 10 corneally blind patients who are not candidates for or have failed one or more corneal transplantations. The KPro had earlier successfully completed a six-month pre-clinical phase proving its safety, and the device is expected to achieve initial clearance in 2022.
According to the World Health Organization, approximately two million new cases of corneal blindness are reported each year, and 30 million people worldwide are legally blind in one or both eyes from corneal injury and disease. A recent study published JAMA Ophthalmology found that the shortage of corneas is around one available cornea for 70 needed. In China, with over five million patients waiting for keratoplasty and only a few thousand transplants a year available, CorNeat is planning a study in 2021 with 60-70 local patients to facilitate turning the CorNeat KPro into a primary solution for corneal blindness, Dr. Litvin says.

“If we look around the world there are about 55 percent of the world population that has no accessibility at all to corneal tissue,” he says. “Every year, the number grows because of this bottleneck created by the gap between the number of people who become blind and the number of people who are treated.”
Sign up for our free weekly newsletter
SubscribeLitvin also notes how in order to properly transplant corneas, ophthalmologists must specialize in corneal transplantation, a procedure that takes at least a year or two to learn. Additionally, once a cornea is harvested, ophthalmologists have only one week to implant it, whereas CorNeat’s technology has a shelf life of two years.
Litvin said that the corneal surgeons at Beilinson Hospital felt completely confident in performing CorNeat’s procedure after just a two-day training session.
“We are delighted to take an active part and be the first to implant CorNeat Vision’s novel synthetic cornea,” said Professor Irit Bahar, director of the Ophthalmology Department at Beilinson Hospital, in the July company release. “The technology behind this implant, which enables to permanently and bio-mechanically attach synthetic materials to live human tissue, is key in turning the tide on global corneal blindness. The fact that this new device integrates with the eye wall also enables an aesthetic solution as it includes a lens which closely resembles the original cornea.”
Additional trials are expected to launch later this year in eight leading hospitals in Canada, the United States, France, China and the Netherlands, the company says.
Professor David Rootman, a world-renowned Canadian ophthalmologist who has trained nearly a hundred cornea specialists around the world said CorNeat Vision’s implant “is poised to revolutionize corneal transplantation.”
“Given the implant’s superior optical quality, the simplicity of its implantation, and its integration concept, the CorNeat KPro is expected to gradually erode the use of human tissue for some corneal indications once retention is proved. This new solution is completely synthetic and does not rely on donor tissue which can carry a virus or any other disease – a key differentiator during this COVID-19 crisis which greatly impacted the availability of corneal tissue,” he added.
CorNeat’s Glaucoma solutions
In addition to the KPro, CorNeat will also begin clinical trials later this year on the CorNeat EverPatch, the first synthetic and non-degradable tissue substitute for ophthalmic surgeries. The EverPatch replaces the use of human tissue and degradable collagen patches for covering and concealing implants like glaucoma drainage devices and for mending traumatic breaks. The EverPatch is composed of a non-woven, polymer matrix that imitates the extracellular matrix, stimulating cellular colonization and integration with the surrounding tissue.
According to Litvin, irreparable damage to the eye’s integrity makes direct and immediate closure impossible, which makes patching the area with preserved and processed tissue the only treatment option. The EverPatch uses inert and non-degradable material that is easy to handle and suture, reducing operating time and eye bank costs.
In addition to the EverPatch, CorNeat has also developed the eShunt, a solution for those who suffer from glaucoma. Glaucoma is a disease of the eye’s optic nerve that occurs when fluid pressure builds up in the anterior chamber of the eye as a result of excess fluid, or the aqueous humor. The eShunt works to regulate intraocular pressure while addressing the shortcomings of alternatives like laser surgery, incisional surgery, and glaucoma drainage devices.
“Glaucoma currently lacks a very efficient solution either surgical or medical. All solutions are only partial and give only some form of pressure-lowering effect but not comprehensive enough,” Dr. Litvin says.
SEE ALSO: NovaSight Raises $8M For ‘Pivotal’ Lazy Eye Treatment Device Study
The eShunt consists of three parts: the inlet, which mimics the pressure regulation mechanism of eye tissues called the trabecular network; the outlet, which is positioned in the intraconal space to absorb drained aqueous humor; and the tube, which biologically integrates with neighboring tissue. The eShunt has successfully passed initial bench tests and animal trials demonstrating seamless integration and an efficient procedure taking less than ten minutes, and the R&D and preclinical phases are expected to take 12-15 months, Dr. Litvin indicates.
Additionally, Litvin tells NoCamels that CorNeat has registered five patents on its technology, including one in dental medicine, an area that also relies heavily on tissue substitutes.
Simply put, “we aim to create implants that restore or mend the eye in a way that restores vision,” says Litvin. The company’s solutions harness “a specific technological ability that we developed that allows us to biointegrate synthetic materials within our own human tissue in a seamless fashion, not causing any inflammatory rejection.”
Related posts
Editors’ & Readers’ Choice: 10 Favorite NoCamels Articles

Forward Facing: What Does The Future Hold For Israeli High-Tech?

Impact Innovation: Israeli Startups That Could Shape Our Future




Facebook comments